The two men were biking together when a car came out of nowhere and hit one of them, killing him.
The second biker was left physically unscathed, but he was severely traumatized, having watched his best friend encounter a fatal accident right in front of him. PTSD, flashbacks, sleeplessness, and anxiety plagued him for years—he couldn’t escape the memory of that tragedy—and it didn’t seem to be abating. He was suffering and he’d tried conventional treatments: psychotherapy, meditation, medication, etc. But nothing seemed to be helping.
That’s when his therapist suggested trying psychedelic-assisted therapy. Following research from places like the Multidisciplinary Association for Psychedelic Studies (MAPS), this emerging form of medicinally enhanced psychic treatment is rapidly gaining momentum and popularity (“Shattering the psychedelic taboo,” 11/11/21).
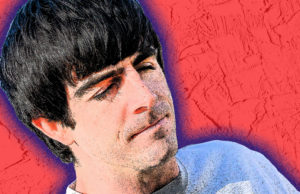
He agreed, found Daniel McQueen with the Center for Medicinal Mindfulness, and signed up for several sessions at the Boulder-based clinic.
“He was able to come away with a lot of personal resolution and acceptance,” McQueen, who has over 20 years of transformational and healing arts experience, recalls. “It was healing his own trauma, but also addressing the grief over the loss of his friend. And then also stepping into the transpersonal realm of spirituality and understanding his relationship to the world in a way that felt really meaningful for him.”
The man’s PTSD symptoms waned over numerous sessions. And when he completed his final one, McQueen says the patient had faced his trauma and worked through those knots that conventional therapy hadn’t been able to untangle.
“It’s not always easy, but it’s always worth it,” he says. “There’s incredible gifts in the transformational process of waking up to yourself.”
It’s just one success story of many that sticks out in McQueen’s mind. His center was one of the first clinics of its kind of to open up in this state and in the entire country. They’ve learned a lot over those years, he says, refining their treatment programs as they did. Currently, the Center for Medicinal Mindfulness offers both cannabis-assisted and ketamine-assisted psychotherapy; it offers private sessions or retreats, group sessions, training, and community events. They’re not just spreading the benefits of psychedelic therapy, they’re working hard to educate and enlighten people about it, as well.
“These medicines, ketamine and cannabis, are very emotionally supportive and positive experiences,” McQueen says. “Even hard [traumatic] material feels really ‘held’ and emotionally supported.”
McQueen has had an interest in psychedelic medicine since he was a teenager, he says. He studied transpersonal therapy at Naropa, and has been working with legal, medicine-enhanced therapy for many years. He started the Center for Medicinal Mindfulness in Boulder in 2012 following the legalization of cannabis, and has been helping people work through their own traumas using the powers of psychedelic medicine ever since.
In 2019 he published a book, Psychedelic Cannabis: Breaking the Gate, where he details his process of using cannabis as a full-blown psychedelic medicine. It involves a specific blend of cannabis, “subjective-dosing,” meditation, music, and of course, guidance. All of which is built in to the program at the Center for Medicinal Mindfulness.
“I’m there [during sessions] to help guide people if they get into choppy waters when it comes to addressing their human trauma,” McQueen says.
McQueen will administer the cannabis blend, and set the patients up on a bed with fuzzy blankets and eye-covers.
“People will lie down and I guide them through a general body-scan meditation with eye coverings and music playing,” says McQueen. “Usually within five, maybe ten minutes, the person’s having a full blown psychedelic experience.”
These experiences are shorter than a conventional psychedelic journey like ketamine or psilocybin, McQueen says. If a patient needs to come out, it’s as easy as sitting up and taking the blindfold off.
The setup for McQueen’s ketamine-assisted therapy is similar, he says, though it serves different purposes (and is not as easy to sit up out of).
He explains that cannabis is a very “somatic medicine,” allowing people to dive deeper into their own body and resolve deep trauma. Ketamine by contrast is an anesthetic drug and a very strong dissociative psychedelic that pulls a patient away from the “self.” It can also help to “reset” the patient’s nervous system, according to McQueen.
That contrast is why the two forms of psychedelic-assisted therapy work so well together, and why McQueen integrates both into some patient’s therapy sessions over several weeks or months.
“Sometimes we have protocols where we’ll start with ketamine if somebody is really having a hard time and that’ll help regulate their nervous system,” McQueen says. “Then we’ll do a series of cannabis sessions to help them do the deep dives into the trauma resolution work. Then, at the end of that we’ll reset their nervous system again with another ketamine experience to reorient [them] towards health and wellbeing.”
With more research about psychedelics being done, more benefits being discovered and the taboos surrounding these substances starting to dissolve, psychedelic-assisted therapy centers like the Center for Medicinal Mindfulness will undoubtedly become more prevalent. McQueen says they already have international programs that work with psilocybin and DMT, but they’re waiting for the laws in the U.S. to change before they venture into that territory here.
They’re “one-hundred percent” moving in that direction when they can, McQueen says.
“We’re just in a really unique position to have been working with plant medicine [for so long] already,” he says. It’s a fact that he says he never takes for granted.
“I’m just super fortunate that I get to do the work I do as a legal, psychedelic guide.”