“The thing that I was really amazed by is that nobody ever asked me, ‘Why did you kill yourself?’” Dave tells me as we talk about his attempted suicide that left him dead for somewhere between 10 and 13 minutes in 1994. “Nobody really asked me.”
So I ask him.
“It was like, this is the last thing I’m taking in this world, I’ve had enough. I’d already lived with too much pain,” he says. “I just said no more. I said this is it, I’ve already had enough insults, I don’t like this, I hurt too much, I’ve hurt too long. And it’s not being attended to.”
Everything that had been building all year — his entire life, really — suddenly broke loose, he says. Since then, as Dave has learned to rebuild his life, he’s also learned to not only talk about his experience but ask others about theirs.
“Let them have a good chance to speak honestly and openly about what brought that on,” he says. “People want to talk about it, they really do. It’s no big secret to them, trust me.”
It’s advice I hear over and over throughout the course of researching efforts to prevent suicide: We have to learn to talk about it.
One of the largest barriers to reducing suicide risk is the social and cultural stigma surrounding the topic. Any one person’s suicide can be caused by a complex variety of circumstances and no two situations are the same. Likewise, no one solution fits all to prevent it. Training health and other community professionals — from teachers, to law enforcement, lawyers and judges — in recognizing the warning signs is key in national efforts to reduce suicide risk, as is the availability, accessibility and affordability of mental health care.
Still, a large part of prevention efforts, according to the experts, centers around destigmatizing suicide and mental health issues, and a large part of the destigmatizing process is learning to talk about it, whether that’s in the classroom, at home or in public.
Unfortunately, the topic tends to make us uncomfortable. As a culture we are hesitant to broach the subject, to leave space for people to share their experience, whether they’ve lost someone they love to suicide or have grappled with their own thoughts. As is the case with most stereotypes, the stigma surrounding mental health and suicide starts to break down when we are personally confronted by someone who has experienced it and/or been affected by it.
Most of the people I talked to about their work to prevent suicide have some sort of personal connection to the topic, and each person willingly and thoughtfully shared with me their stories of loss, grief and, ultimately, hope. In truth, I didn’t return the favor.
As I interviewed them, one by one, I was constantly reminded of my own experience and the need to be more honest about it.
 Someone very close to me has struggled with suicidality for the last two decades, and I thought about her a lot while working on this story.
Someone very close to me has struggled with suicidality for the last two decades, and I thought about her a lot while working on this story.
I remember that winter day, driving my normal route, when the phone rang, an unidentified number showing up on the screen. I remember hearing I should probably call the hospital to find out if she was still alive. I remember agonizing over why I hadn’t asked more pointedly how she was doing the last time we talked, less than 48 hours earlier.
It’s only been since this most recent attempt that we really started talking about it, both with each other and other people. It’s becoming a more regular topic of our conversations, whether prompted by a high-profile suicide in the news or simply because it’s time to check in again, ask how she’s doing, what she’s thinking about. It’s rarely an easy conversation, but it is a necessary one.
I find the subject of suicide to be an uncomfortable conversation to have with other people as well. When the topic is mentioned casually in conversation — usually in reference to news headlines — I often sit quietly and let it pass. Many times in those moments I would rather not share my own experiences, afraid not of judgment necessarily, but rather of exposing my own raw emotion. Still, more and more frequently I feel compelled to tell my story, at least in part, in the hopes that perspectives can change, that people unexposed to the realities of suicide and mental illness will see things a little differently than before, that suicide can be destigmatized.
When people interject, which they almost always do, with common misperceptions and/or platitudes about suicide, I often have to steer the conversation away from myself and switch into explanatory mode.
In the United States, almost 45,000 people died by suicide in 2016, according to the Centers for Disease Control (CDC), tenth on the list of leading causes of death after illnesses like heart disease, cancer, influenza and pneumonia, as well as accidents. At the same time, 9.3 million adults have had suicidal thoughts, 2.7 million have made a plan to attempt suicide and 1.3 million adults have attempted suicide. That’s roughly 25 attempts for every completed suicide.
It’s a pandemic that’s getting worse. Between 1999 and 2016, almost every state saw a 30 percent or more increase. Colorado increased by 34 percent and ranked ninth in the nation for highest suicide rates. In 2016, the state saw its highest number of suicides to date, 1,156, according to the Office of Suicide Prevention’s annual report. It was the seventh leading cause of death for Coloradans that year and the leading cause of death for people ages 10-24.
“If you knew there was a bomb going off somewhere in the country every 12 minutes, which is the suicide rate, maybe you couldn’t diffuse them all, but you would certainly try to detect the patterns and try to reach as many as you could before they exploded,” says Andrew Romanoff, president and CEO of Mental Health Colorado, a statewide advocacy organization. “We need to treat this like the crisis it is.”
Romanoff’s cousin died by suicide in the backyard of his house while the rest of the family were inside celebrating New Year’s Day 2015. In her note, Romanoff says, she told the family that she loved them and there was nothing they could have done.
“And then she said, ‘Please tell everybody it was a car accident,’” he says. “My guess is that even in her death, she wanted to preserve her reputation. She didn’t want to be known as someone who was suicidal or depressed or mentally ill so she came up with this cover story, which we couldn’t figure out a way to honor.”
For Romanoff, it’s further proof of the stigma that surrounds mental health and suicide.
“We tell people with mental illness to snap out of it, which is something we would never say to someone with cancer,” he continues. “It’s not a character flaw or a figment of [their] imagination. … It’s an illness, and it’s treatable. Science has increasingly shown that on a neurological, physiological or biochemical basis, but even that we distinguish mental illness from physical illness perpetuates the stigma. It’s a false distinction.”
Mental illness and suicide are often seen as “no casserole” situations, says Susan Marine, who lost both of her children to suicide four years apart. She now works with the Suicide Prevention Coalition of Colorado and is a member of the Suicide Prevention Commission under the Department of Health and Human Services. “If your circle of friends know that your child had their appendix out, your friends are going to bring you casseroles. If they find out your child is seriously depressed they most likely won’t. I still think we have a lot of work to do to get to that point.”
Although often correlated, suicidality is not relegated only to the realm of mental illness. More than half of the people who died by suicide in 2016 did not have a known mental health condition, according to the CDC.
“Anybody can have suicidal thoughts and it could happen because they are experiencing an intense emotion or moment in their life that they are overwhelmed by and it seems like a solution and they don’t have a mental health diagnosis,” says Natalie Trombley a licensed clinical social worker with Mental Health Partners (MHP) working in Boulder and Broomfield counties. “I think that happens far more frequently than anyone is aware of or at least talks about.”
In 2016, 3 percent of deaths in Boulder County were by suicide and in the 10-year span between 2006 and 2016, 683 people completed suicide. This number is the focus of MHP’s new suicide prevention campaign called Be 1 of 4,098, which aims to train 4,098 people in suicide prevention between now and December 2019.
“What we’re trying to do is train as many people as possible that can offer hope through positive action, such as how to approach or talk to a person who is potentially suicidal,” Trombley says. “We have to extend the conversation outside of the field of mental health, to make more people comfortable [with] talking about such a tough topic.”
She likens it to the topic of sexual abuse, a once taboo topic that when undiscussed is often not dealt with. “Then, once that stopped and people starting talking about it, the incidence of sexual abuse declined quite a bit… because people were thinking about it, looking for it, talking about it,” Trombley says. “And this topic is no different.”
She says most people are afraid to broach the subject with people potentially thinking about suicide out of fear — fear of what they may hear or their own inability to help or even that they’ll trigger the act simply by asking about it. “What actually happens is they are likely to feel some relief that you are willing to talk about it and, in turn, the conversation offers the potential for a positive outcome,” she says.
“All the studies say that if somebody is going to complete suicide they’ve already thought about it, so you addressing it with them is not going to push them in that direction. It actually has the opposite effect, it actually helps them, it makes them feel heard, and you can try to get them care,” says Kristina Shaw, marketing director with MHP. “Mental health issues aren’t just mental illness.” More than 80 percent of people experience some sort of mental health issue during their lives, she says. It can take many forms and be something as common as stress.
This is where education is key, prevention experts say, and it’s where most prevention training focuses. By teaching everyone from kids to adults to not only recognize common warning signs of suicide, but also to become comfortable asking friends, family members and coworkers about it, everyone can help break down the stigma that surrounds suicide, removing the cloud of shame that often hovers around it.
“Our mission is to educate so that the kids see that it’s OK to talk about it, that it’s OK to get help,” says Kathy Valentine from Colie’s Closet, a peer-to-peer training program that first started as a fundraising effort by a Fairview High student in response to the suicide of a family member. “Many times there’ll be kids talking about themselves or talking about their friends.”
Over the last three years, peer volunteers with Colie’s Closet have spoken to 9,000 kids throughout Boulder Valley School District about depression and suicide awareness, how to spot warning signs and what to do if a student or one of their friends is feeling this way. The hope is that by normalizing the conversation around suicide and mental health, suicide itself won’t become so common. And the only way to normalize the conversation is to continue having it.
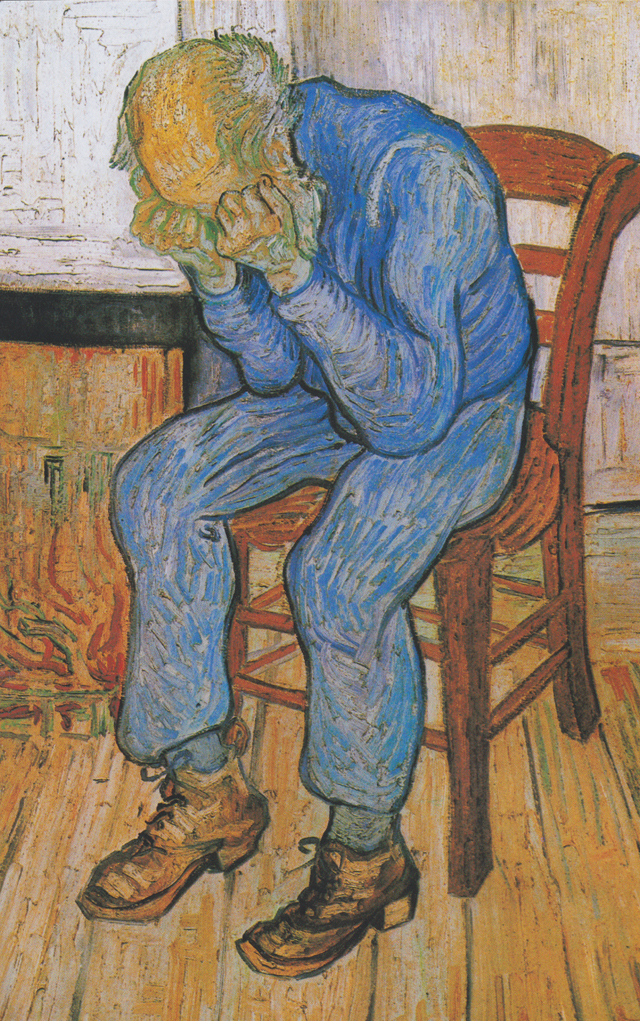
“We don’t have an easy way to talk in our culture about illness or pain or that life is hard sometimes. We have this sort of cheerful, optimistic, pull-yourself-up-by-your-bootstraps expectation that everything can be solved,” says Joy Redstone, a social worker and addictions counselor at Naropa who lost her husband four years ago to suicide. “And sometimes people’s pain doesn’t need to be solved, it just needs to be heard or witnessed or shared with someone else.”
The choice to listen, and not necessarily respond, can be scary. In my case, it comes with the uncertainty that one of the people closest to me may try again and we might not be so lucky next time. It can be painful to hear her say she’s having a hard day, or she’s overwhelmed, or even that she wishes she had been successful.
As much as I want to say, “Please don’t do that to us,” I know that’s not helpful. That sort of sentiment does nothing to break down the shame and stigma around suicide. All it does is refocus the conversation around me instead of giving her the space to say whatever she needs to say, to let her be heard. Instead, I’m learning to listen, empathizing with her, recognizing that her experience in this world, living every day with mental illness, is something I may never fully understand. But I’m trying. I’m listening.
“It matters that somebody gives a shit,” Dave tells me at the end of our conversation.”It really does matter that somebody actually cares.”
If you or someone you know is in crisis please call the state hotline at 1-844-493-TALK or 8255.
For a free mental health screening visit mentalhealthcolorado.org. For more information about the variety of suicide prevention efforts, including trainings and support groups for survivors, going on around Boulder County visit hopecoalitionboulder.org.