Theresa Halsey, a member of the Hunkpapa Lakota tribe and producer of the Indian Voices radio show on KGNU, has been dealing with diabetes for a couple of decades. In 2000, she decided to visit Denver Indian Health and Family Services to get tested. That’s where her journey with the Special Diabetes Program for Indians (SDPI) began.
Through SDPI, Halsey attends classes for diabetes management. She learns how to navigate the produce section of the grocery store and how to cook vegetables. She sees what healthy portion sizes look like, and she gets to participate in monthly challenges that promote healthy living. For November, she’s vowed to drink water every day — no sugary drinks allowed.
Halsey insists SDPI has helped her adopt healthier habits in her and her children’s lives. Yet, as much of an impact as this program might have in bettering her health, the federal government has been less than enthusiastic when it comes to acknowledging its significance.
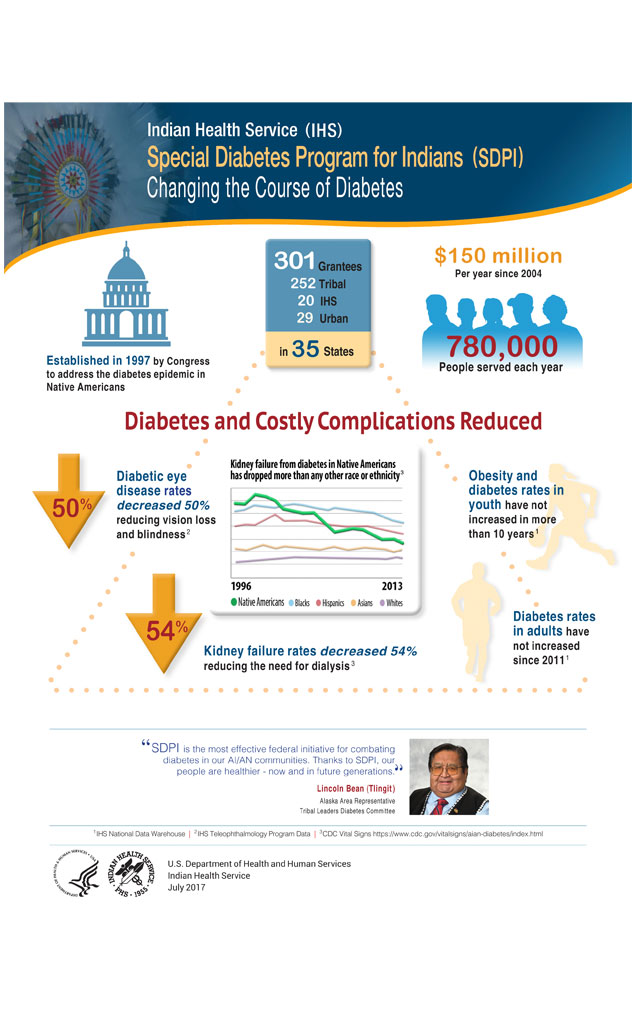
In October, Congress renewed funds for SDPI, but only until Dec. 31. Despite the program’s success, renewal periods only last months at a time between Congressional debates regarding its funding. While the current state of government support looks bleak, researchers at the University of Colorado’s Anschutz Medical Campus and members of the SDPI community are committed to making sure the Native voice isn’t lost.
“People need to be lobbying their states because that’s where the actual money will be coming down from; not that much money is coming from the [federal] government,” Halsey says.
According to the National Indian Health Board, current costs for diabetes in Colorado total around $3 billion. Even so, the state’s SDPI program receives only $900,000 to fund Denver Indian Health and Family Services, Ute Mountain Tribe and the Southern Ute Tribe.
The program is facilitated by the federal Indian Health Service (IHS), an agency within the Department of Health and Human Services. The agency works through a network of hospitals and clinics, many of which facilitate SDPI.
This chronically underfunded agency originates from the nation’s earliest treaty agreements established in 1787, according to the department’s website. Yet, Native American health care too often sits on the backburner of the government’s to-do list. Historically, tribes have argued that the federal government has violated many treaty provisions, as evidenced most recently by last year’s Standing Rock protests against the controversial Dakota Access Pipeline, which threatens the Standing Rock Tribe’s water supply. IHS’s lack of funding may well be viewed as yet another outgrowth of these violations.
This poses a problem for Native Americans seeking diabetes programs since IHS has little money to work with. Sparse funding leads to limited options for programs, which dissuades many Native Americans from getting help.
According to the First Nations Development Institute, 68 percent of Native Americans live on or near their home reservation in rural areas that often lack adequate medical facilities. Sparsely populated areas such as these are often overlooked by government and corporations that fund the healthcare system.
With the nearest reservation in Colorado about seven hours away from Denver, many of the state’s Native Americans struggle to find the same quality of medical care as their urban counterparts.
“At the funding level — the federal level, they don’t care,” Halsey says. “They don’t care about the poor, they don’t care about the young, they don’t care about the old. They don’t care.”
However, Native Americans are two times more likely to develop type two diabetes than any other subsect of the population, according to the Centers for Disease Control. Despite the dramatic disparity, the general public remains ignorant of the problem.
Dr. Spero Manson, a Chippewa from Turtle Mountain Reservation and the research director at Anschutz’s Center for American Indian and Alaska Native Health, says that even his colleagues within the program aren’t aware all of the issues that plague Native communities.
“They’re stunned by the extent of discrimination that our people experience,” Manson says. “It’s just not even on the radar screen for them. These are colleagues whom I work with who are studying these matters. Think about how that multiplies when you go out into the broader community.”
Manson has spent his career researching the potential solutions to the problems Native communities face and learning how to apply them in the areas of need. One of his first exposures to the disparity between Native Americans and the rest of the population came during a 1970s study that found a link between combat and post-traumatic stress disorder (PTSD). Native soldiers were not included in the study, preventing them from receiving government aid for PTSD.
The diabetes epidemic within the Native community shares the same disparity today. But a huge part of SDPI’s success revolves around uniting the Native community and creating a positive environment for each patient.
“I think [Native Americans] really like that we talk about traditional food practices and the role of historical trauma in the development of diabetes,” says Sarah Hormachea, a registered dietician and certified diabetes educator for Denver’s SDPI chapter. “I think it would be harder to have those discussions in a heterogeneous class.”
Manson refers to this as the collective genius. Bringing together Native Americans to share lessons of success makes SDPI an important program. Creating positive communities like this is crucial, given centuries of discrimination and poor living conditions.
Manson insinuates that diabetes may be a symptom of the trauma many Native Americans still face today. His 2005 study found that they “witnessed traumatic events [and] experienced traumas more often than the U.S. population as a whole.”
Halsey can attest to this research. She credits her development of diabetes to her traumatic experience at a boarding school for Native Americans.
Over the course of several years in a South Dakota boarding school, Halsey was starved, received poor treatment from teachers and was forced to do work around the school. While she managed the trauma of boarding school, she says that many of her classmates continue to struggle with the experience.
“A lot of my friends have gone on to the spirit world already because of all the problems,” Halsey says. “It’s not because they’re alcoholics, it’s not because they do drugs — those are the symptoms. The [cause] is intergenerational trauma.”
Halsey has always been a fighter, though. She describes standing up to the teachers for her younger siblings, something that was unthinkable in boarding school. “I’ve always been advocating for myself and others,” she says.
SDPI hopes to expand its program in Denver to continue improving the health of Colorado Native Americans. But the age-old narrative of Native Americans against the government is never far away as Congress is continuously unwillingness to provide ample, long-term funding to the program.
If history has taught us anything, it is that the Native community is willing to fight for its rights and is in it for the long haul.