A cancer diagnosis is a heavy reality, no matter what type or which stage. More than a quarter of patients surveyed by the American Cancer Society report suffering from depression and end-of-life anxiety.
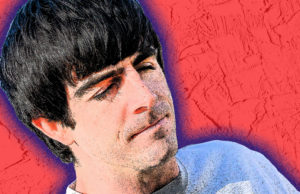
“We also have a patient population that [doesn’t fall] into the realm of anxiety and depression, but their functional status deteriorates so significantly because of the emotional hit that they’re suffering from,” says Dr. Moran Amit, a head and neck surgeon and assistant professor at the University of Texas (UT) MD Anderson Cancer Center. “They’ve just been traumatized by their cancer diagnoses or cancer treatment.”
Currently, the majority of such cases are referred to cognitive behavioral therapy (CBT) and are sometimes prescribed either a selective serotonin reuptake inhibitor (SSRI) or a benzodiazepine. But Amit says many cancer patients he sees are resistant to CBT, or cannot muster the energy or find the time to fully invest in it. Benzodiazepines are highly addictive, Amit adds, and both those and SSRIs should be prescribed carefully and in low doses to cancer patients.
Amit believes the medical community needs another tool to help patients cope. He’s in the process of setting up a clinical trial to observe how psilocybin affects the brains of people living with different types of cancer. He and his colleagues at UT want to know whether or not this psychedelic molecule might be a viable alternative to established remedies.
“I became familiar with the hallucinogenic drugs family, most of which affect different types of serotonin receptors,” Amit says. “And those have been shown, at least in the lab with animals, to change those neurons a little bit.”
He references numerous studies that have indicated this. One, published in theNew England Journal of Medicine in 2021, made direct clinical trial comparisons between psilocybin and established treatments for depression, like SSRIs. It concluded that there was no “significant difference in antidepressant effects” between psilocybin and SSRIs, and that secondary outcomes “generally favored psilocybin.”
Another from 2016 found that one-time use of psilocybin produced clinically relevant and long-lasting effects on depressive and anxious symptoms. The scientists concluded that psilocybin is “an alternative to first-line antidepressants.”
“The beauty of psilocybin is that the effect is durable,” Amit says. “With SSRIs, I need to keep my patients on them in order to maintain the effect. But with psilocybin and drugs from the same family, you see a [lasting] effect only after one or two sessions.”
With colleagues Dan Yaniv, Lois Michelle Ramondetta and Lorenzo Cohen, Amit co-authored a commentary in the International Journal of Gynecological Cancer pleading with their peers to explore the use of psilocybin with cancer patients.
“Considering the prevalence of distress among … cancer patients and the potential benefits and safety of psychedelics, there is a clear need for more well-designed protocols prioritizing safety and exploring psilocybin, and other psychedelics, in this vulnerable population,” the authors write.
Amit says patients in his upcoming clinical trial will prepare for psilocybin-assisted psychotherapy for several weeks before ingesting anything. At the end of the third week, participants will undergo a psilocybin treatment with integration sessions following the experience. Subjects will repeat the process at six weeks. Amit’s team will analyze MRI scans before and after treatment to see how it affects brain neuroplasticity. Patients will be monitored throughout the process.
“My fulfillment, or sense of joy, is with my ability to make [this treatment] accessible to our patients,” Amit says. “This is a drug that, in your wildest dreams, you would have never imagined we’re going to give [to people] in Texas. But we’ve made it accessible for patients. I’m really happy about it.”
Amit encourages cancer patients suffering from depression or anxiety to contact him at [email protected].